COLOSTOMY
Procedure overview
A colostomy is an operation that creates an opening for the colon, or large intestine, through the abdomen. A colostomy may be temporary or permanent. It is usually done after bowel surgery or injury. Most permanent colostomies are “end colostomies,” while many temporary colostomies bring the side of the colon up to an opening in the abdomen.
During an end colostomy, the end of the colon is brought through the abdominal wall, where it may be turned under, like a cuff. The edges of the colon are then stitched to the skin of the abdominal wall to form an opening called a stoma. Stool drains from the stoma into a bag or pouch attached to the abdomen. In a temporary “loop colostomy,” a hole is cut in the side of the colon and stitched to a corresponding hole in the abdominal wall. This can be more easily reversed later by simply detaching the colon from the abdominal wall and closing the holes to reestablish the flow of stool through the colon.
Reasons for the procedure
Colostomy surgery may be needed to treat several different diseases and conditions. These include:
- Birth defect, such as a blocked or missing anal opening, called an imperforate anus
- Serious infection, such as diverticulitis, inflammation of little sacs on the colon
- Inflammatory bowel disease
- Injury to the colon or rectum
- Partial or complete intestinal or bowel blockage
- Rectal or colon cancer
- Wounds or fistulas in the perineum. A fistula is an abnormal connection between internal parts of the body, or between an internal organ and the skin. A woman’s perineum is the area between her anus and vulva; a man’s lies between his anus and scrotum.
The reason for the colostomy helps the healthcare provider decide whether it will be short-term or permanent. For example, some infections or injuries require giving the bowel a temporary rest, then reattaching it. A permanent colostomy may be required for a more serious or incurable problem, such as cancer that requires removal of the rectum, or a failure of the muscles that control elimination.
How the digestive system works
A colostomy won’t change the way your digestive system works. Normally, after you chew and swallow your food, it goes through your esophagus, or swallowing tube, into your stomach.
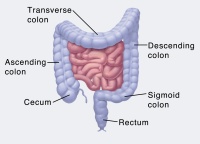
From there, it travels to your small intestine and then to your large intestine, or colon. Hours or days later, the indigestible residue leaves the storage area of your rectum via your anus, as stool. Stool typically stays loose and liquid during its passage through the upper colon. There, water is absorbed from it, so the stool gets firmer as it nears the rectum.
The ascending colon goes up the right side of your body. The stool here is liquid and somewhat acidic, and it contains digestive enzymes. The transverse colon goes across your upper abdomen, and the descending and sigmoid colon go down the left side of your body to your rectum. In the left colon, the stool becomes progressively less liquid, less acidic, and contains fewer enzymes.
Where your colon is interrupted determines how irritating to the skin your stool output will be. The more liquid the stool, the more important it will be to protect your abdominal skin after a colostomy.
Risks of the procedure
Getting a colostomy marks a big change in your life, but the surgery itself is uncomplicated. It will be performed under general anesthesia, so you will be unconscious and feel no pain. A colostomy may be done as open surgery, or laparoscopically, via several tiny cuts.
As with any surgery, the main risks for anesthesia are breathing problems and poor reactions to medications. A colostomy carries other surgical risks:
- Bleeding
- Damage to nearby organs
- Infection
After surgery, risks include:
- Narrowing of the colostomy opening
- Scar tissue that causes intestinal blockage
- Skin irritation
- Wound opening
- Developing a hernia at the incision
Before the procedure
If possible, be sure to discuss your surgical and postsurgical options with a doctor and an ostomy nurse (a nurse who is specially trained to help colostomy patients) before surgery. It may also help to meet with an ostomy visitor. This is a volunteer who has had a colostomy and can help you understand how to live with one. And, before or after your surgery, you may wish to attend an ostomy support group. You can find out more about such groups from the United Ostomy Associations of America or the American Cancer Society.
During the procedure
Depending on why you need a colostomy, it will be made in one of 4 parts of the colon: ascending, transverse, descending, or sigmoid.
- A transverse colostomy is performed on the middle section of the colon, and the stoma will be somewhere across the upper abdomen. This type of surgery–often temporary–is typically performed for diverticulitis, inflammatory bowel disease, cancer, blockage, injury or a birth defect. In a transverse colostomy, the stool leaves the colon through the stoma before reaching the descending colon. Your stoma may have one or two openings. One opening is for stool. The second possible stoma is for the mucus that the resting part of your colon normally keeps producing. If you have only one stoma, this mucus will pass through your rectum and anus.
- An ascending colostomy goes on the right side of your abdomen, leaving only a short part of the colon active. It is generally performed only when blockage or severe disease prevents a colostomy further along the colon.
- A descending colostomy goes on the lower left side of the abdomen, while a sigmoid colostomy–the most common type–is placed a few inches lower.
After the procedure
You may be able to suck on ice chips on the same day as your surgery. You’ll probably be given clear fluids the next day. Some people eat normally within two days after a colostomy.
A normal stoma is moist and pink or red colored. When you first see your colostomy, it may appear dark red and swollen, with bruises. Don’t worry. Within a few weeks, the color will lighten and bruises should disappear.
The bandage or clear pouch covering your colostomy right after surgery probably won’t be the same type that you’ll use at home. Your colostomy will drain stool from your colon into this colostomy pouch or bag. Your stool will probably be more liquid than before surgery. Your stool consistency will also depend on what type of colostomy you have and how much of your colon is still active.
In the hospital
A colostomy requires a hospital stay of about 3 days to a week. Your stay will probably be longer if the colostomy was performed for an emergency. During your hospital stay, you’ll learn to care for your colostomy and the appliance or pouch that collects your stool.
Your nurse will show you how to clean your stoma. After you go home, you’ll do this gently every day with warm water only. Then gently pat dry or allow the area to air dry. Don’t worry if you see a little bit of blood.
Use your time in the hospital to learn how to care for your colostomy. If you have an ascending or transverse colostomy, you will need to wear a slim, lightweight, drainable pouch at all times. There are many different types of pouches, varying in cost and made from odor-resistant materials.
Some people with a descending or sigmoid colostomy can eventually learn to predict when their bowels will move and wear a pouch only when they expect a movement. They may also be able to master a process called irrigation to stimulate regular, controlled bowel movements.
Before going home, be sure to talk with an ostomy nurse or other expert who can help you try out the equipment you’ll need. What works best will depend on what type of colostomy you have; the length of your stoma; your abdominal shape and firmness; any scars or folds near the stoma; and your height and weight.
Sometimes, the rectum and anus must be surgically removed, leaving what’s called a posterior wound. In the hospital, you’ll use dressings and pads to cover this wound, and you may also take sitz baths–shallow, warm-water soaks. Ask your doctor and nurse how to care for your posterior wound until it heals. If problems should occur, please contact your doctor.
At home
The skin around your stoma should look the same as elsewhere on your abdomen. Exposure to stool, especially loose stool, can be irritating. Here are some tips to protect your skin:
- Make sure your pouch and skin barrier opening are the right size.
- Change the pouch regularly to avoid leakage and skin irritation. Don’t wait until your skin begins to itch and burn.
- Remove the pouching system gently, pushing your skin away instead of pulling.
- Barrier creams may be used if the skin becomes irritated despite these measures.
Notify your doctor to report any of the following:
- Cramps that last more than two hours
- Continuous nausea or throwing up
- Bad or unusual odor for more than a week
- Change in your stoma size or color
- Blocked or bulging stoma
- Bleeding from the stoma opening or in the pouch
- Wound or cut in the stoma
- Serious skin irritation or sores
- Watery stool for more than five hours
- Anything unusual that concerns you
A good rule is to empty your pouch when it’s one-third full. And be sure to change the pouch before it leaks. As a general rule, change it no more than once a day, but not less than every three or four days.
A colostomy represents a big change, but you will soon learn to live with it. Even though you can feel the pouch against your body, no one else can see it. Do not feel the need to explain your colostomy to everyone who asks; only share as much as you want to.